The Central Leadership Role of the Developmental Neuro Pediatrician: Dr Kondekar Santosh, Autism doctor Mumbai, emphasises
The Central Leadership Role of the Developmental Neuro Pediatrician
A Strong Clinical Perspective on Why Coordinated Developmental Care Must Be Medically Led
Introduction
Children grow through a complex process of brain development that influences movement, language, cognition, behavior, emotions, and social interaction. When concerns arise — whether subtle or obvious — timely and correctly guided intervention can significantly change the child’s trajectory.
Yet developmental care is often fragmented, with therapies running in parallel without central clinical leadership. This is where the Developmental Neuro Pediatrician becomes indispensable — not merely as a diagnostician, but as the architect, coordinator, analyst, and decision-maker guiding the child’s developmental roadmap.
This article presents a strong clinical perspective: developmental care achieves optimal outcomes only when centrally led by a developmental neuro pediatrician with continuous reassessment and goal redirection.
Who First Notices Developmental Concerns
Concerns may be identified by:
Parents or caregivers
Nursery or school teachers
Counselors or principals
Pediatricians or therapists
NICU or hospital teams
They may notice differences compared to peers in:
Developmental milestones
Communication
Behavior
Academic performance
Social interaction
Early recognition matters because a developing brain has high plasticity, and delays left unaddressed may evolve into disability.
Why Early Evaluation Matters
Hidden causes of developmental difficulties may include:
Nutritional deficiencies such as iron deficiency
Hormonal disorders like thyroid dysfunction
Sequelae of birth injury
Genetic conditions
Developmental disorders
Seizure disorders
Neurological diseases not yet clinically obvious
Identifying these early allows targeted treatment and better outcomes.
Core Responsibilities of a Developmental Neuro Pediatrician
1️⃣ Detailed History and Clinical Examination
The first step is a comprehensive evaluation that includes:
-
Pregnancy and birth history
-
Developmental milestones
-
Medical history
-
Family history
-
Behavioral observations
-
Neurological examination
This helps build a full picture of the child’s developmental profile.
2️⃣ Confirmation and Classification of the Problem
The specialist determines:
-
Whether the child truly has a delay or disorder
-
The type of condition (e.g., autism, ADHD, global delay, learning disorder)
-
Severity and functional impact
Accurate classification guides appropriate intervention.
3️⃣ Planning Investigations if Needed
Not every child requires tests, but when indicated they may include:
-
Hearing and vision testing
-
Blood tests (nutritional, metabolic, hormonal)
-
Genetic testing
-
EEG
-
Neuroimaging
Investigations aim to identify treatable causes.
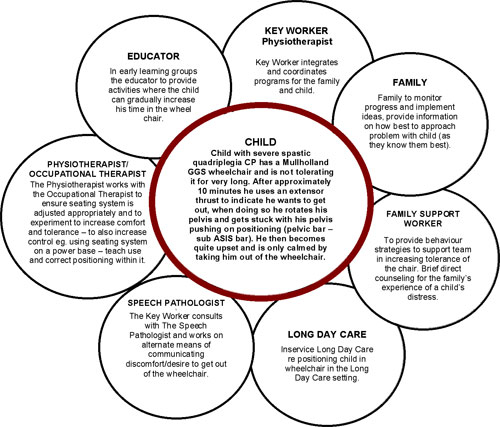
4️⃣ Creating a Multidisciplinary Referral Plan
Developmental care is team-based. The neuro pediatrician decides:
-
Which therapies are needed
-
Priority of therapies
-
Frequency of sessions
-
Goals of intervention
This ensures coordinated and efficient care.
5️⃣ Pharmacotherapy When Required
Medications may be used for:
-
ADHD
-
Behavioral regulation
-
Sleep problems
-
Seizures
-
Mood or anxiety symptoms
The goal is always to improve function and therapy participation.
6️⃣ Certification and Documentation
The specialist provides:
-
Diagnostic reports
-
Disability certification when applicable
-
School recommendations
-
Therapy plans
This documentation helps families access services and support.
7️⃣ Monitoring Progress and Reassessment
Development is dynamic. Regular follow-ups help:
-
Track improvements
-
Identify new concerns
-
Adjust therapy plans
-
Monitor medication effects
8️⃣ Revising Plans to Keep the Child “Therapy-Able”
The neuro pediatrician ensures the child remains ready to benefit from therapy by addressing:
-
Behavior challenges
-
Attention issues
-
Medical problems
-
Sleep difficulties
9️⃣ Holistic and Medico-Legal Responsibility
They take overall responsibility for:
-
Coordinating care
-
Ensuring appropriate referrals
-
Ethical decision-making
-
Documentation
-
Long-term developmental planning
🔟 Counseling Families and Explaining Prognosis
One of the most important roles is helping families understand:
-
The child’s condition
-
Expected outcomes
-
Realistic goals
-
Therapy expectations
-
School planning
-
Transition planning
This empowers parents to become active partners in care
The Core Difference: Therapist vs Development Architect
Therapists are domain experts focusing on specific skills.
The developmental neuro pediatrician integrates all domains, understands brain maturation timelines, identifies barriers, and adjusts the roadmap.
👉 Therapists build skills. The developmental pediatrician designs the developmental trajectory.
Superior Role in Coordination
A child rarely has a single isolated issue.
The developmental pediatrician:
Aligns therapy goals
Prevents conflicting approaches
Ensures appropriate sequencing
Avoids therapy overload
Maintains functional focus
Without this coordination, therapies risk becoming fragmented.
Identifying Missing Links
When progress is slow, the key question is WHY.
The developmental pediatrician evaluates for:
Attention dysregulation
Sleep problems
Sensory dysregulation
Nutritional deficiencies
Subclinical seizures
Emotional dysregulation
Cognitive limitations
Weak receptive foundation
These hidden barriers often explain lack of progress despite therapy.
Detecting and Managing Comorbidities
Developmental disorders frequently coexist with other conditions such as:
Autism with ADHD
ADHD with learning disorder
Speech delay with hearing impairment
Behavioral issues with sleep disorder
Medical insight is essential to manage these interactions effectively.
Directing Therapy Goals
Therapists depend on clarity regarding priorities.
The developmental pediatrician ensures goals are:
Developmentally appropriate
Sequential
Brain-ready
Functional
Time sensitive
This prevents working on skills before foundational readiness.
Continuous Decision-Making and Revision
Development is dynamic.
The developmental pediatrician:
Reviews responses frequently
Identifies plateau early
Modifies therapy intensity
Adds or stops interventions
Adjusts goals
Therapy plans must evolve continuously.
Importance of Frequent Monitoring
Frequent reviews help:
Detect subtle progress
Prevent wrong direction
Optimize therapy timing
Provide feedback to therapists and educators
They guide what to continue, modify, or stop.
Guiding Domain Priority
Each therapist naturally focuses on their domain.
But development follows hierarchy.
The developmental pediatrician decides:
Which domain is foundational
What to prioritize
When to shift focus
When integration is required
Correct sequencing accelerates progress.
Turning the Child Therapy-Able
A child may not progress because they are not ready to benefit from therapy.
The developmental pediatrician prepares the brain by improving:
Attention
Regulation
Receptivity
Sleep
Emotional stability
Behavioral control
Accelerating Developmental Velocity: Dr Kondekars Concept
When clinically appropriate, interventions may include:
Nutritional optimization
Targeted supplements
Medical treatment
Behavioral regulation strategies
The aim is improving learning efficiency and developmental rate.
Why Therapists Alone Cannot Replace This Role
Even highly skilled therapists:
Do not manage medical contributors
Do not evaluate comorbid neurodevelopmental biology
Do not revise global developmental strategy
Do not determine domain priority
Do not manage medications
This reflects complementary roles — not hierarchy of skill — but leadership must be centralized.
Coordinating Therapies
The developmental pediatrician guides referrals to:
Speech therapy
Occupational therapy
Behavioral therapy
Physiotherapy
Special education
Vision, hearing, nutrition, endocrine, orthopedic care
Referrals are not the end of care — reassessment within 1–3 months is essential if progress is inadequate.
The Developmental Pediatrician as Navigator
Therapists are skilled professionals, but the developmental pediatrician interprets the developmental map, trajectory, and timing.
Without navigation, effort may not lead to optimal outcomes.
Strong Clinical Opinion
Developmental care without central medical leadership risks becoming fragmented, delayed, inefficient, and sometimes misguided.
The developmental neuro pediatrician provides:
Neurobiological understanding
Longitudinal perspective
Clinical decision authority
Integration across domains
Continuous recalibration
This leadership transforms therapy from activity into progress.
Regular developmental pediatrician follow-ups should be considered essential, not optional, in any child receiving developmental interventions.
Key Messages
⭐ Developmental care must be medically coordinated
⭐ Domain priority determines efficiency
⭐ Frequent reassessment prevents stagnation
⭐ Therapy readiness determines outcomes
⭐ Comorbidities must be actively managed
⭐ Goals must remain dynamic
Conclusion
The developmental neuro pediatrician plays a uniquely comprehensive role — combining medical expertise, developmental science, and strategic coordination.
Their leadership ensures therapies are biologically informed, time-sensitive, and continuously optimized.
When this model is followed, developmental trajectories improve, families feel guided, and therapy becomes purposeful rather than fragmented.
Ultimately, the mission remains clear:
⭐ To help every child reach their fullest developmental potential through coordinated, evidence-informed, and continuously guided care.
References
American Academy of Pediatrics Council on Children With Disabilities. Identifying infants and young children with developmental disorders in the medical home. Pediatrics. 2020.
Hyman SL, Levy SE, Myers SM. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics. 2020.
Shevell M et al. Practice parameter: evaluation of the child with global developmental delay. Neurology. 2003.
Lipkin PH, Macias MM. Promoting optimal development: identifying infants and young children with developmental disorders. Pediatrics. 2020.
Johnson CP, Myers SM. Identification and evaluation of children with autism spectrum disorders. Pediatrics.
Thapar A, Cooper M. Attention deficit hyperactivity disorder. Lancet. 2016.
Shonkoff JP, Phillips DA. From Neurons to Neighborhoods: The Science of Early Childhood Development. National Academy Press.
Dawson G et al. Early behavioral intervention is associated with normalized brain activity. Journal of the American Academy of Child & Adolescent Psychiatry.
Guralnick MJ. Early intervention approaches to enhance development. Pediatrics.
World Health Organization. Nurturing Care for Early Childhood Development Framework.

Comments
Post a Comment
https://speechandsenses.blogspot.com/p/httpsspeechandsenses.html read before you comment